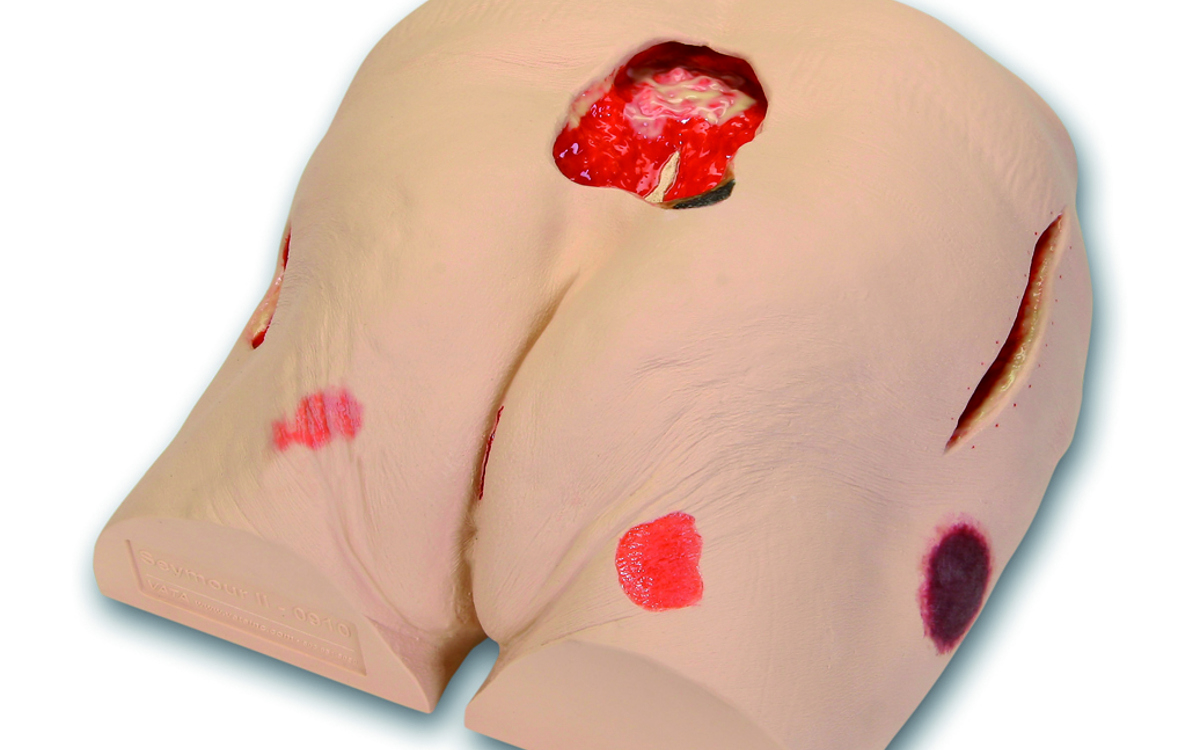








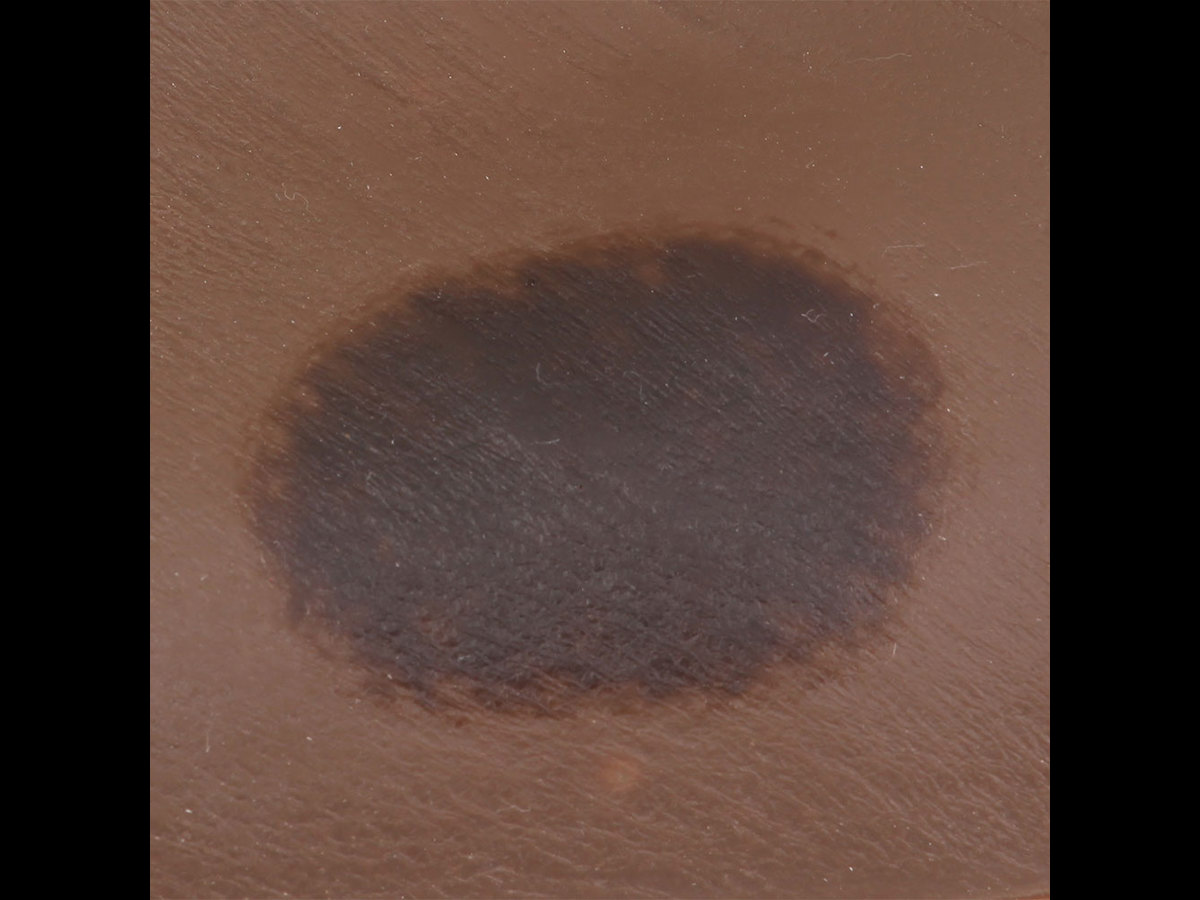
Seymour II Wound Care Model™ - Dark
Skin Tone
Please note: VATA Inc. products are currently not available for purchase in Canada.
Based on a 74-year-old patient, this model aids in the identification and assessment of wounds. Once the different aetiologies are understood, this model can be used to discuss and devise treatment plans.
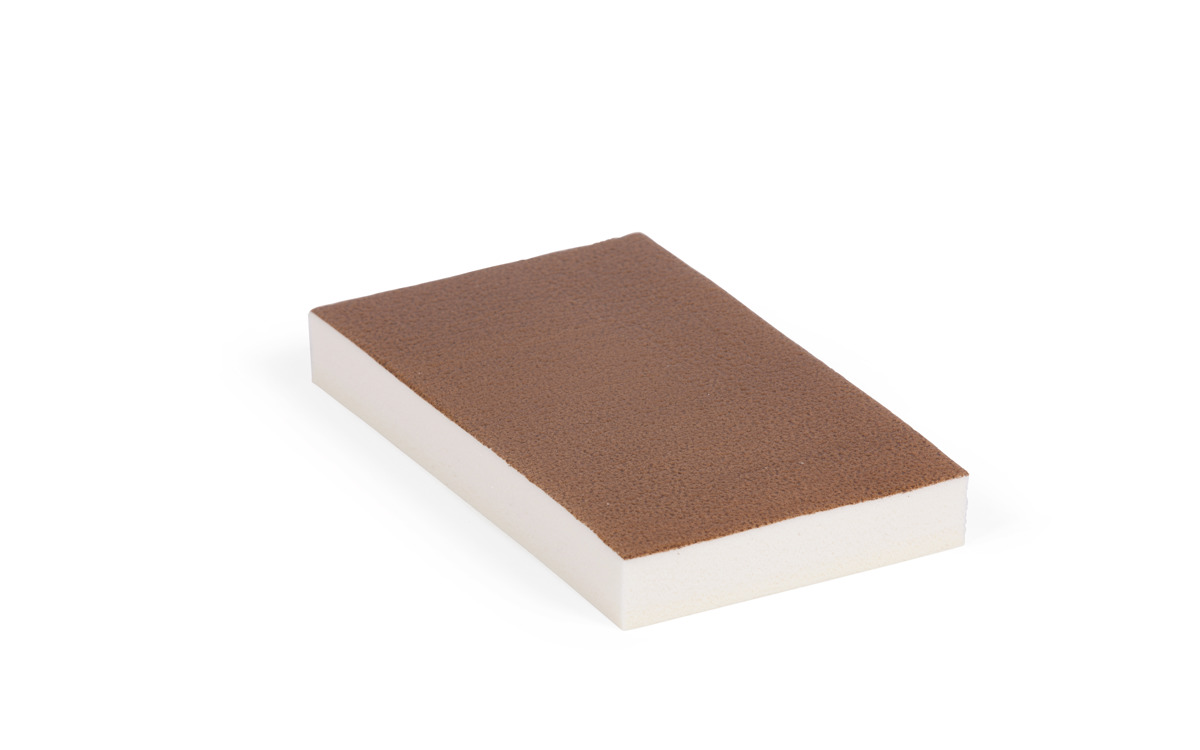
Realism
- Unique flexible life-like material permits the placement of dressings
- For use with negative pressure wound therapy devices (without adhesive residue)
Cleaning
- Washable with soap & water
Anatomy
- Displays the following conditions:
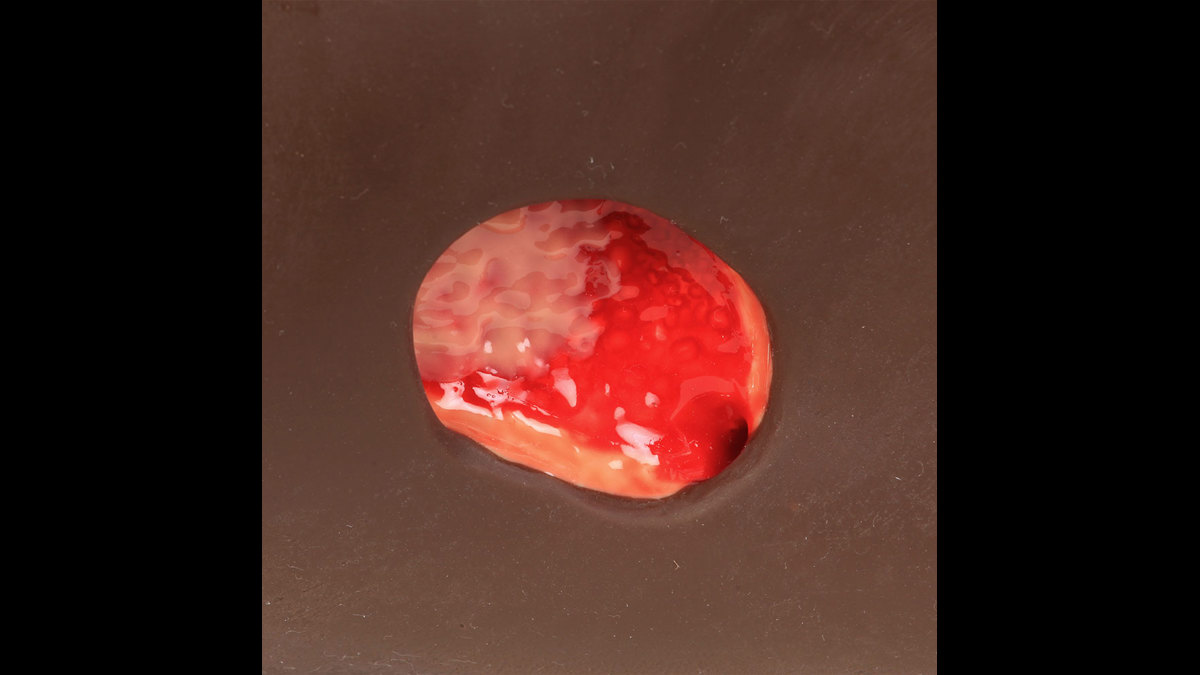
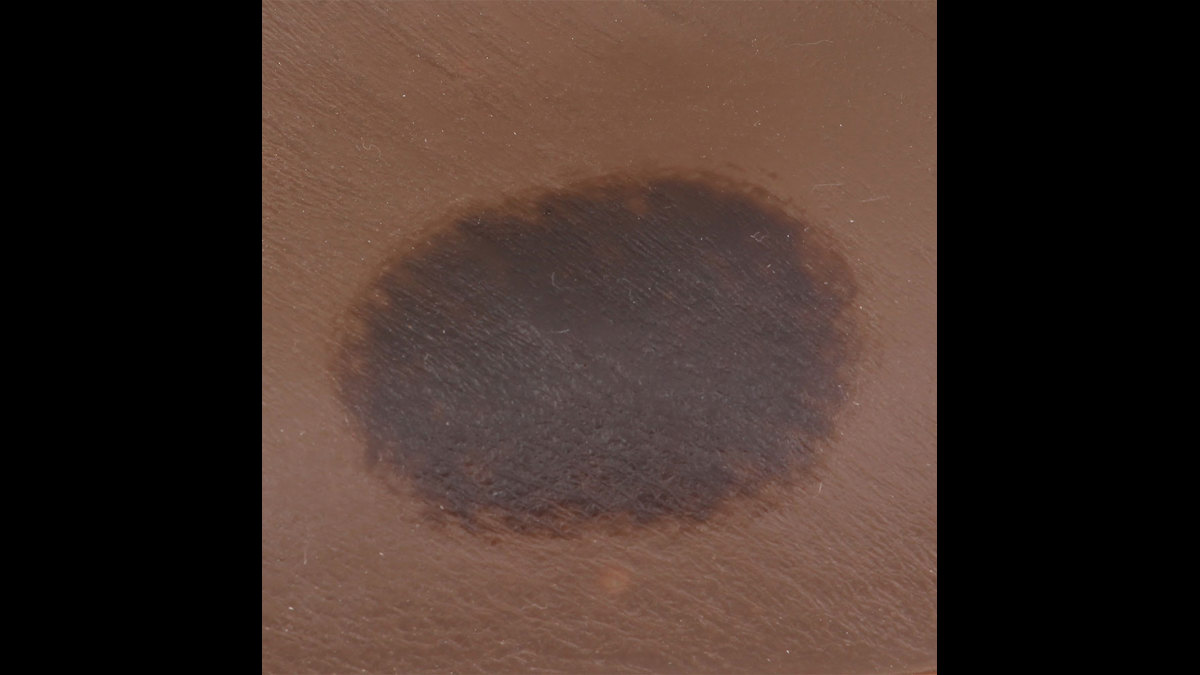
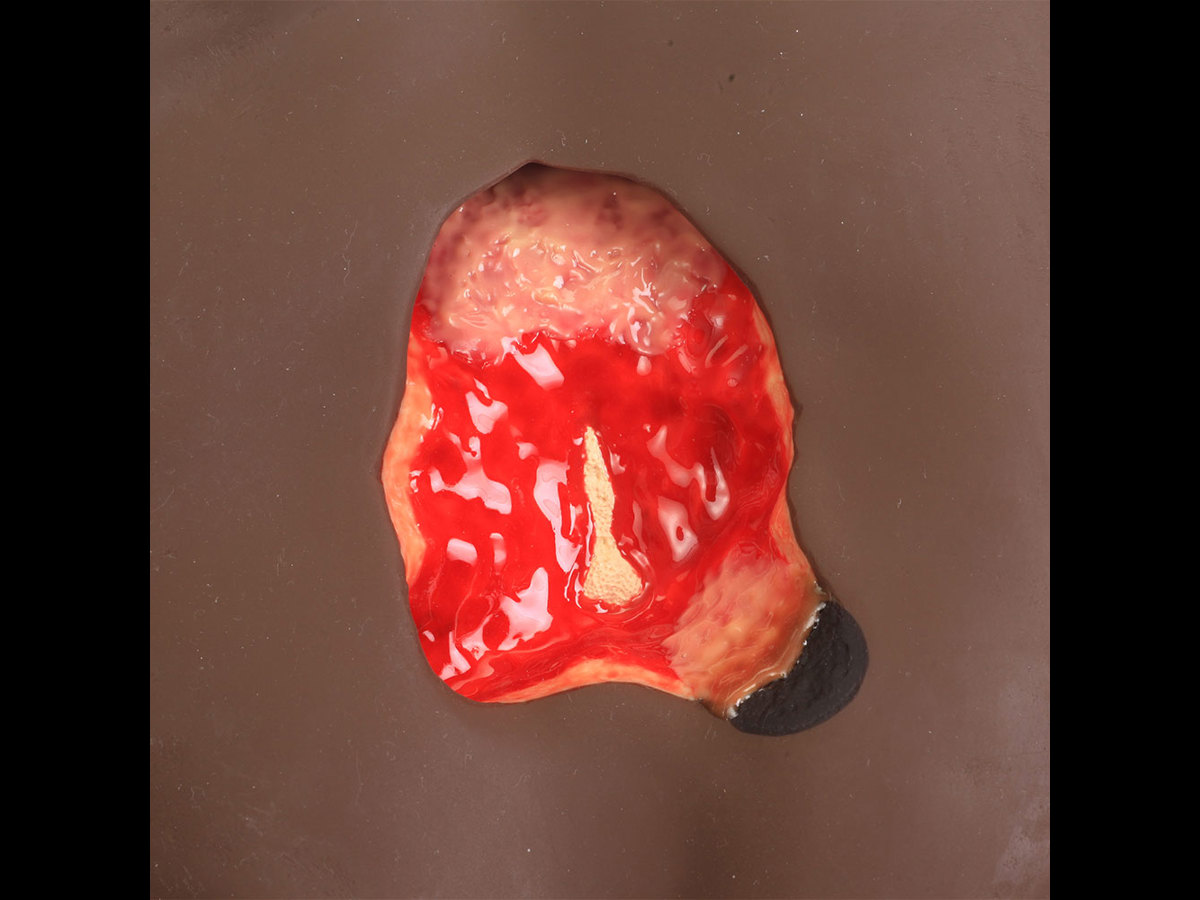
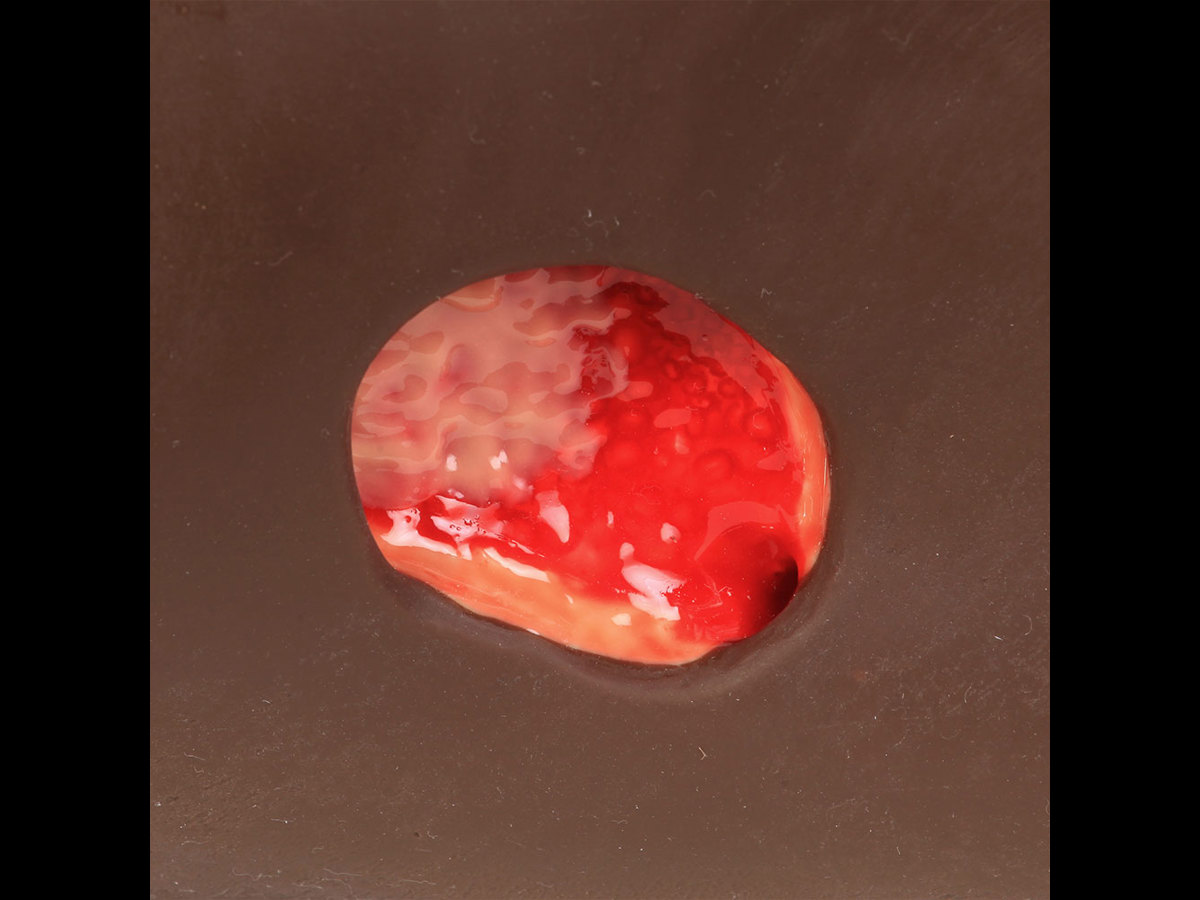
- Stage 1 pressure ulcer
- Stage 2 blister intact
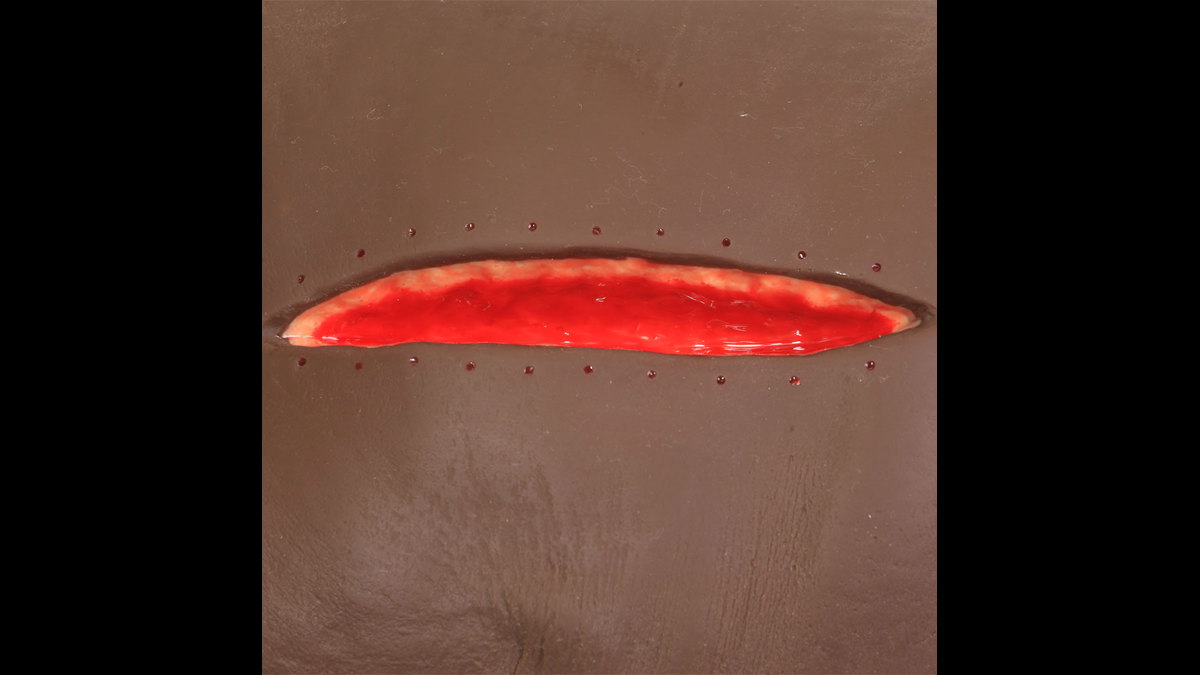
- Stage 3 pressure ulcer with undermining, tunnelling, subcutaneous fat and slough.
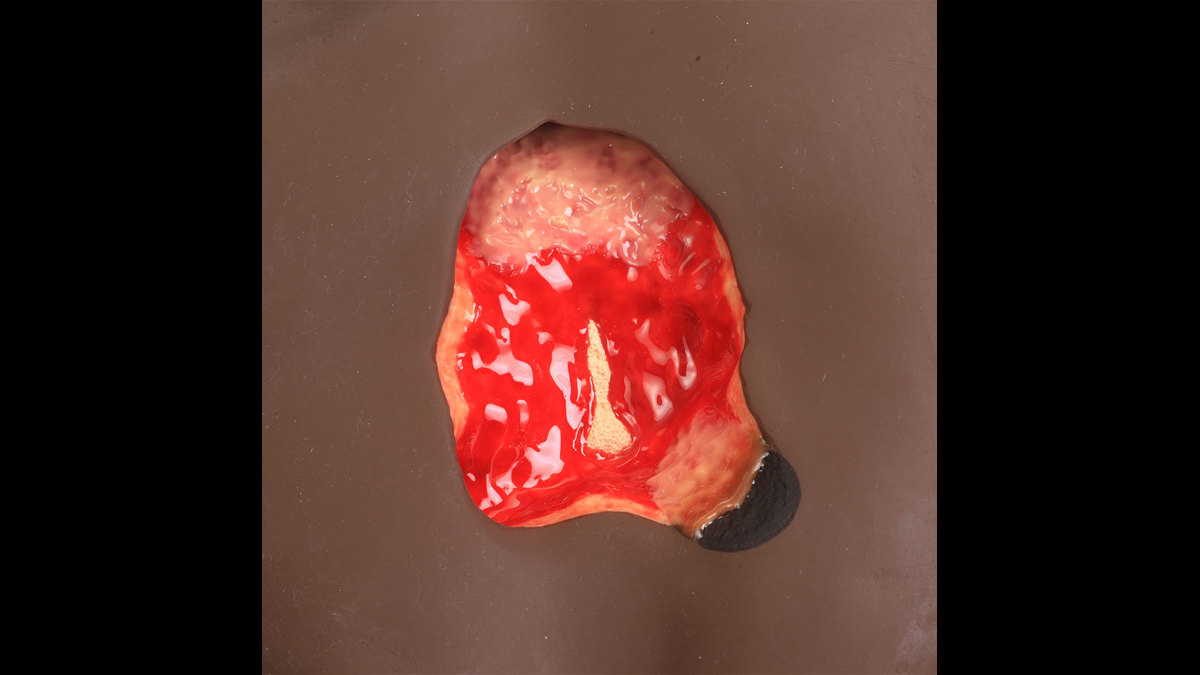
- Stage 4 deep ulcer with exposed bone, undermining, tunnelling, subcutaneous fat, eschar & slough.
- Suspected DTI, unstageable & a 5 1/2” dehisced wound.
Skills Gained
- Skills assessment
- Competency testing
- Dressing techniques
- Negative wound therapy
- Measurement of wound length, depth, undermining and tunneling
Product Contains
Works with the following products:
References
AAFP Recommended Curriculum Guidelines for Family Medicine Residents, Care of Older Adults Reprint No. 264, p.5 15.Care of conditions that are common in older adults... k. Dermatologic: xerosis, cutaneous neoplasms, environmental and traumatic lesions including skin tears and pressure ulcers, wounds, skin manifestations of systemic illness
AAMC Recommendations for Clinical Skills Curricula for Undergraduate Medical Education (2005, p. 30): General wound care technique; Wound debridement, simple
NMC Standards of Proficiency: (p. 28). undertake wound care including dressings, suture removal, and vacuum closures using aseptic techniques and apply pressure bandaging *AH *CH
Paramedics Australasia: Paramedicine roles: General Care Paramedic: Specialist management of wounds (cleaning, closure and dressing)
Undergraduate Nursing - Australian Wound Mangement Association "Standard 4: Clinical Decision Making: Practice. Wound Management is practised according to the best available evidence for optimising outcomes for the individual, their wound and their healing environment."
Competence and Curriculum Framework for the Physician Assistant 2012, p 23 2.6.3 The Physician Assistant should be familiar with the following patient presentations and should be able to manage and diagnose: Skin changes: colour, ulceration, pruritis, rashes
Specialty Training Curriculum for Core Medical Training, 2013 p.105: Recognise life threatening skin rashes presenting with ulcers, commence treatment and involve senior; Recognise the importance of prevention of pressure ulcers and diabetic ulcers
Practical Skills and Procedures, General Medical Council, April 2019, p.6 Therapeutic Procedures 21. Carry out wound care and basic wound closure and dressing. Provide basic care of surgical or traumatic wounds and apply dressings appropriately.
NMC Future nurse: Standards of proficiency for registered nurses, 17 May 2018, p.34 4.1 observe, assess and optimise skin and hygiene status and determine the need for support and intervention 4.2 use contemporary approaches to the assessment of skin integrity and use appropriate products to prevent or manage skin breakdown 4.4 identify and manage skin irritations and rashes 4.6 use aseptic techniques when undertaking wound care including dressings, pressure bandaging, suture removal,and vacuum closures 4.7 use aseptic techniques when managing wound and drainage processes