News
Simulation Based Education In Pharmacy Programs
14 September 2021
Simulation in healthcare education is now accepted as a viable method of teaching individuals as well as teams’ ways to improve patient outcomes through safer care. Many medical specialty governing bodies have moved from recommending simulation-based education to mandating the addition of simulation to curricula. However, there is a growing trend for slightly more prescriptive recommendations, such as the U.S. Accreditation Council for Pharmacy Education (ACPE) standards, which recommend “the use of SBE in interprofessional team education and introductory pharmacy practice experiences (IPPE) to mimic realistic patient care situations (Accreditation Council for Pharmacy Education, 2015)” in Doctoral Pharmacy programs.1 With this recommendation, programs seeking accreditation began to think of innovative ways that they could participate in interprofessional simulation scenarios. Seybert et.al (2019) from the University of Pittsburgh school of Pharmacy published an article related to their integration of simulation, with results showing “improvement in learner satisfaction, knowledge enhancement, critical thinking skills, and problem-solving in patient care topics.”2
In London, Kayyali et.al (2019) used interprofessional education (IPE) simulation with nursing and pharmacy students to prepare for expanding role demands from healthcare services. Results of the study not only showed an increased appreciation for new roles, communication, and teamwork skills, but students also “recognised the importance, usefulness and need for IPE.”3
In the UK and Scotland, there is a push for pharmacists to be highly involved in patient education about managing their medications through a vision called “prescription for excellence”, where an aging population is able to live longer, healthier lives at home.4 While pharmacy schools have “increased their clinical and patient-related content, there is an urgent need to develop this further, especially with respect to the interdisciplinary elements necessary for pharmacists to establish themselves as an effective part of the healthcare team”.4 One of the biggest challenges that pharmacy programmes face is the placement of pharmacy students in clinical areas, which are “extremely limited” creating “a situation which is already recognised as having a negative impact on the development of the skills new pharmacists will need in practice, including communication, conflict resolution, adaptability and the ability to “think on one’s feet”.4 It is now believed that simulation can be used to bridge this gap in clinical placement, decrease the high incidence of medication errors, increase the appreciation of the pharmacist role as a member of the healthcare team, and ultimately improve the overall education, confidence, and satisfaction of the pharmacy student.
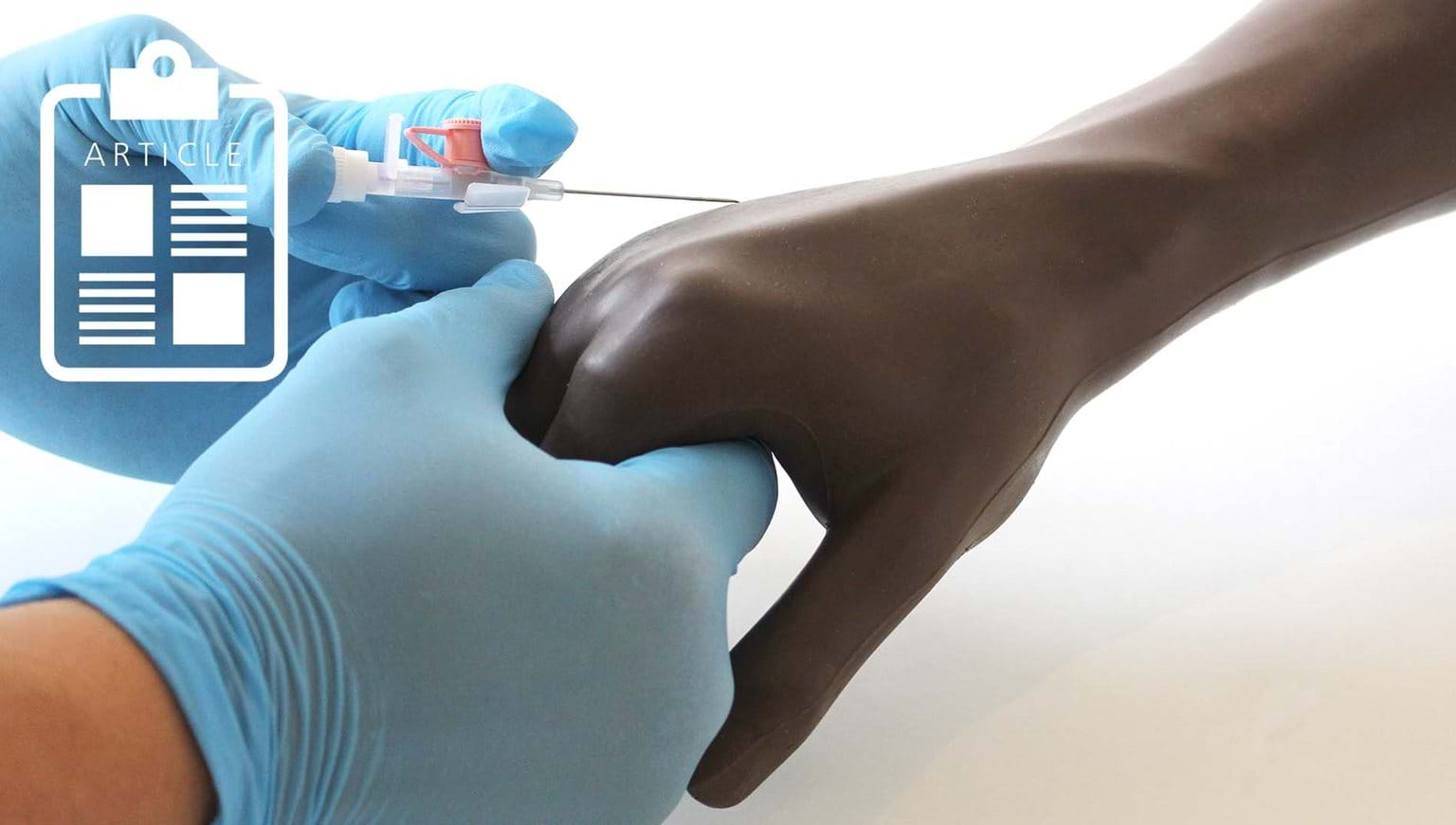
At Limbs & Things, we support the concept of interprofessional education through team training. We not only provide anatomically correct models for procedural skills, but many also include the ability to perform hybrid scenarios using simulated patients which can increase the focus communication skills for the healthcare team, including pharmacists, who are crucial in the education of patients about medication safety. Working together, the whole team can continue to improve patient outcomes. For more information on any of our hybrid models, contact our team here.
1 Integrating simulation into advanced pharmacy practice experience curriculum
2 Evidence for Simulation in Pharmacy Education
3 Simulation in pharmacy education to enhance interprofessional education
4 Pharmacy Simulation: A Scottish, Student-Led Perspective with Lessons for the UK and Beyond


