The Importance of Training in Chest Tube Placement
Read this article to understand the significance of chest tube placement training and the trauma scenarios that require this skill.
Breathing is an involuntary action that maintains a balance of oxygen and carbon dioxide in your system. Most of the time, you don’t really think about breathing, because your brain is subconsciously doing the work for you. If carbon dioxide begins to build up in your system, your brain tells you to breathe deeper, or faster.
When you feel short of breath for any reason, breathing becomes a conscious effort. The most common time this occurs is with exertion, which could mean anything from climbing a flight of stairs for some to running a marathon for others. There are, however, more serious conditions that cause shortness of breath that can be very scary. One of these conditions is a collapsed lung, or pneumothorax.
Defined, a pneumothorax occurs “when air leaks into the space between your lung and chest wall”1 (called the pleural space). “This air pushes on the outside of your lung and makes it collapse. A pneumothorax can be a complete lung collapse or only a portion of the lung.”1
Pneumothorax is diagnosed in the following ways:
- Primary spontaneous pneumothorax (PSP): “air in the pleural space without clinically apparent underlying lung disease,”2 often without any prior symptoms of illness.
- Secondary spontaneous pneumothorax (SSP): a spontaneous pneumothorax “with underlying lung disease including cystic fibrosis, chronic obstructive pulmonary disease (COPD), AIDS, etc.”2
- Tension pneumothorax: “pneumothorax with significant respiratory or hemodynamic compromise that reverses on decompression (needle or finger) alone.”2
- Iatrogenic pneumothorax: “a traumatic pneumothorax that results from injury to the pleura, with air introduced into the pleural cavity secondary to diagnostic or therapeutic medical intervention.”3
Although mild cases may go away with minimal treatment, it is not uncommon that both adult and pediatric patients might need a chest tube (also called a chest drain) to resolve a pneumothorax. “According to the literature, Chest drains were needed for more than two million adults in the United States (US) for one year... Furthermore, In the United Kingdom (UK), during a six-month period in one hospital, there were 375 children who had an inserted chest drain. Moreover, about 25% of all major trauma patients admitted to trauma centers in Australia needed chest drain.”4
Courses in trauma care globally, including the Advanced Trauma Life Support (ATLS) and the European Trauma Course (ETC), stress the importance of both needle decompression and chest tube placement (also called thoracostomy) for critically injured patients in the field. Additionally, many patients in hospital Emergency departments and Intensive Care units require placement of chest drains. For this reason, many medical specialties are trained in this procedural skill.
Since the chest tube must remain in place until the fluid, blood, or air has completely drained from the pleural space, patients are often placed in routine medical-surgical units once they are stable. This requires ongoing nursing care that some nurses do not feel qualified to provide. Globally, research has shown that nurses have “insufficient knowledge of chest drain care,”4 ranging from 22% to 85% of the studied samples.4 This insufficiency in training may lead to preventable complications for the patient.

Training for the placement and ongoing care of chest tubes must be a multi-disciplinary endeavor. While placing the chest tube is certainly a learned skill, ongoing care can be frightening and cumbersome for nursing staff.
Training for care of chest tubes should begin in nursing school, but it should not end there. Any nurse in an acute care setting may be assigned a chest tube patient. Therefore, nurses should have access to ongoing education, not only about assisting with insertion, but also dressing changes, suction, milking of the tube when a clot is present, clamping, and removal of the tube.
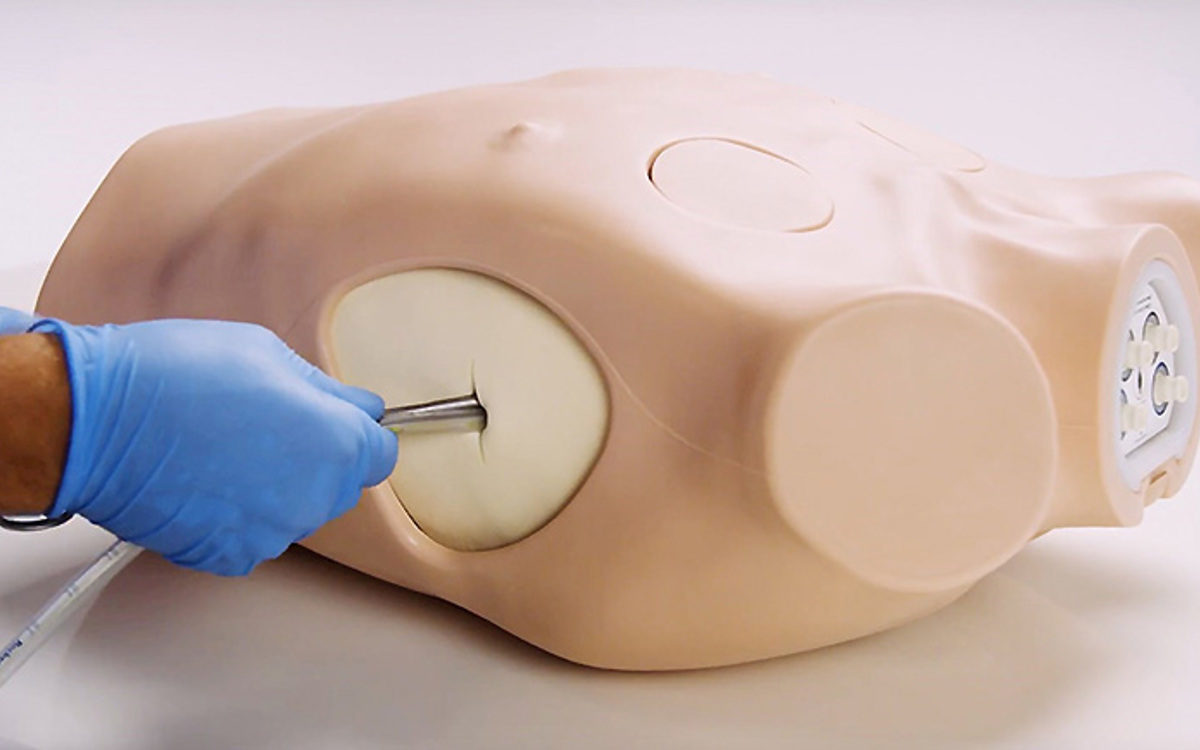
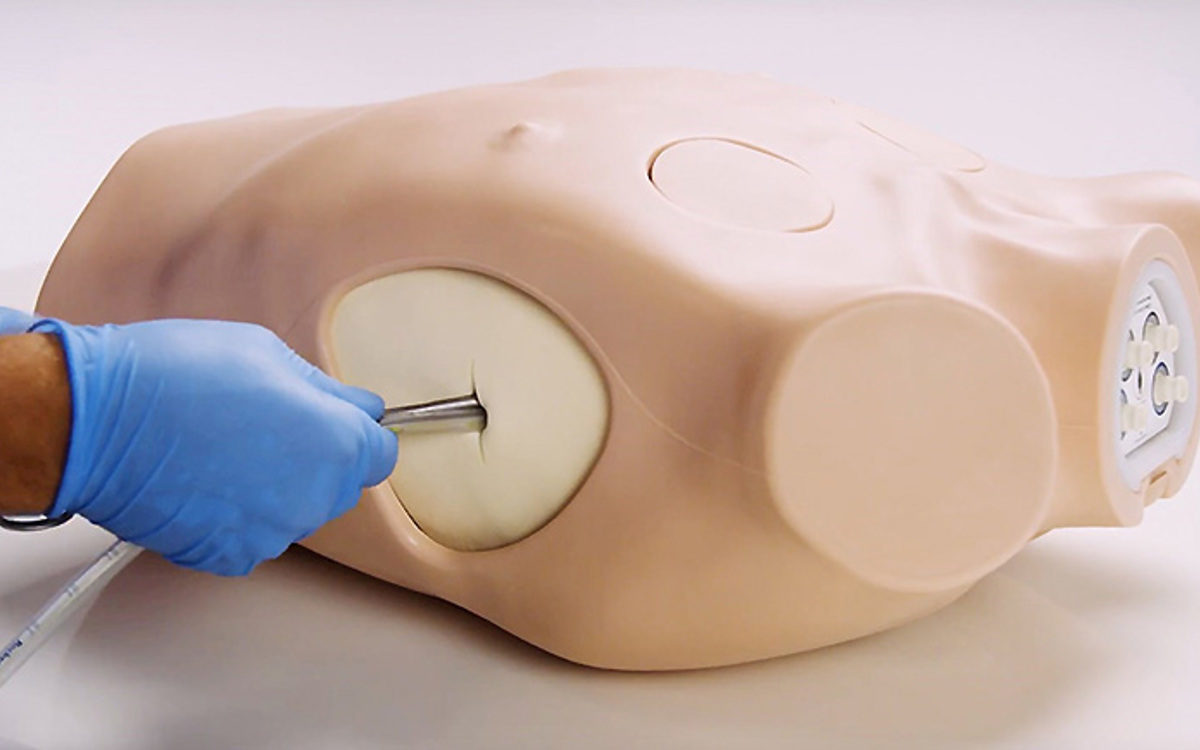
The Limbs & Things Chest Drain and Needle Decompression Trainer is the ideal simulator to deliver training in both surgical, guidewire assisted thoracostomy and thoracentesis, as well as the ongoing care and removal of chest tubes.
Featuring bone and soft tissue landmarks and internal ultrasound anatomy, this model is approved by the American College of Surgeons (ACS) for delivering the ATLS 10th edition course. Not only can it be used to simulate chest tube insertions (including the landmark and ultrasound guided Seldinger techniques), chest drainage, and needle decompression techniques, its flexibility and portability allows for training nursing staff in the ongoing care and removal of an inserted tube.
References:
Did you like this article?
Remember to share on social media and tag us!