Breaking Down Barriers in Life-Saving Care of Women
Although the risk of a cardiac event is similar in both genders, women experiencing cardiac arrest are significantly less likely to receive bystander CPR.

A recent study published in BMC Cardiovascular Disorders has shed more light on a troubling reality in emergency medicine: although the risk of a cardiac event is similar in both genders, women experiencing cardiac arrest are significantly less likely to receive bystander CPR.
The study states the disparity stems from hesitation around physical contact and concerns about removing clothing during resuscitation.
From the four hundred participants responding, more men than women, and even medical students trained in CPR expressed hesitation due to lack of confidence and practical experience with diverse anatomical presentations.
The new article reiterates that when seconds count in cardiac emergencies, any hesitation can mean the difference between life and death, and that the barriers faced can be overcome with proper training.
The Training Gap
The study found that most participants had never practiced CPR on a female manikin, despite widespread support for including them in training programs. This creates a dangerous disconnect: people learn life-saving techniques on male models, then face uncertainty when encountering different anatomy in real emergencies.
However, the encouraging results show that proper training can eliminate these barriers. Among participants who had received comprehensive CPR training, many of the gender-based differences disappeared entirely, proving that education truly works when it addresses real-world scenarios.
Beyond Emergency Response
This challenge extends beyond bystander CPR into clinical settings where healthcare students, residents, and professionals must perform many examinations and procedural skills, requiring confidence and competence regardless of patient gender, yet some training programs fail to adequately prepare learners for this reality.
Over the past 10 years, modern medical education has begun to fully embrace equity, inclusion, and diverse training solutions that directly address real-world challenges.
Specialized equipment now allows students and healthcare providers to practice essential skills across different anatomical, generational, and cultural presentations, building both competence and confidence.
Limbs & Things is working to develop innovative training products that tackle many educational gaps head-on. As our research and development and product management teams were laying the groundwork for what would eventually become the CaRE (Cardiovascular and Respiratory Exam) Trainer, it became increasingly apparent that the examination of women was seen to be a barrier for students learning the procedures.
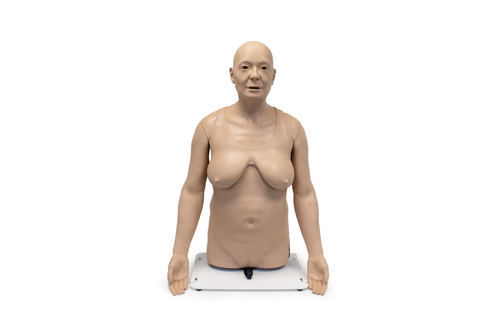
A very important part of the cardiovascular examination of a woman requires uncovering the chest area and moving the breasts. Students must learn to approach this with sensitivity and clear communication. Additionally, those with acute or chronic cardiovascular conditions do not appear as fit, young, strong, healthy white males.
For these reasons our medical artist used three-dimensional scans and extensive reference materials to create a sculpt for the CaRE body that shows real and realistic features: an older, culturally diverse person with scars, wrinkles, and sagging skin in all the right places. She also sculpted a female version of the same body, with realistic breasts for her age.
Our team spent a long time considering the correct materials to best imitate the fall and weight of the breast tissue to get as close to real life as possible. This laid the groundwork for a new direction for our medical sculpting work: closer to a real patient, closer to life where it matters.
Other Limbs & Things products that meet diverse and equitable training needs include the CFPT (Clinical Female Pelvic Trainer), which creates safe learning opportunities for intimate exams, allowing students to work through initial discomfort in a controlled educational environment before encountering real patients.
This kind of preparation builds the professional demeanor essential for quality patient care. Additionally, our Breast Examination Trainer can be worn by Simulated Patients, and both male and female learners to help in the understanding of how to communicate properly while conducting an exam that could be uncomfortable for both the provider and the patient.
Other products that promote examination while protecting the privacy of female patients include the female catheterization trainers, the female pelvic ultrasound phantom , as well as full body manikins, all providing multiple opportunities for learning procedures while gaining confidence in skills related to unique considerations increasingly recognized in women's healthcare.
The Professional Development Factor
The newest study reiterates that comprehensive training can overcome cultural barriers and personal hesitation. When people receive proper education using diverse anatomical models, they develop what educators call "professional identity” - the confidence to provide excellent care based on medical need rather than personal comfort levels.
This professional development does not happen automatically. Students need explicit practice with realistic scenarios, different skin colors to represent cultural sensitivities that may need to be highlighted, open discussions about potential challenging situations, and repeated exposure that builds both skill and confidence.
Gender and cultural disparities in healthcare are not inevitable. They are training gaps that we can address through better educational approaches that prepare healthcare providers for the real world they will face.
References:
- Cheng W, Liu J, Zhou C, Wang X. Factors analysis of lower probability of receiving bystander CPR in females: a web-based survey. BMC Cardiovascular Disorders. 2025;25:270.
- Blewer AL, McGovern SK, Schmicker RH, et al. Gender disparities among adult recipients of bystander cardiopulmonary resuscitation in the public. Circulation: Cardiovascular Quality and Outcomes. 2018;11(8):e004710.
- Kramer CE, Wilkins MS, Davies JM, et al. Does the sex of a simulated patient affect CPR? Resuscitation. 2015;86:82-7.
Did you like this article?
Share it on social media today and remember to tag us!

