Assisted Vaginal Births
A push to re-introduce the use of assisted or operative vaginal delivery has developed after a global increase in C-sections. Read more here.
Assisted vaginal birth (AVB), also referred to as Operative vaginal delivery (OVD) “refers to a vaginal birth conducted with the help of an instrument, such as a forceps or a vacuum extractor (VE)”.2 “Common indications for AVB include prolonged second stage, maternal exhaustion or medical indications (e.g., maternal heart disease), and suspected or confirmed fetal compromise in the second stage of labour.”2
“Although the World Health Organization (WHO) statistics have estimated that about 68% of births occur naturally, operative vaginal delivery remains at a fairly high level and represents about 10% in the UK, 3% in the USA.”1 Contraindications for assisted vaginal delivery include an “unengaged fetal head, unknown fetal position, preterm pregnancies of < 34 weeks, and fetal bleeding disorders.”1
Even though the thought of forceps or a vacuum extractor can be daunting for the laboring woman, when “compared with second stage C/S, AVB is associated with lower risks of haemorrhage, postoperative infection, faster maternal recovery, shorter hospital stays and cost-savings for health systems. Moreover, women are more likely to have a spontaneous vaginal birth in their next pregnancy after an AVB than after a C/S.”2
“The benefits associated with AVB may be greater in low-resource settings where many births occur in primary care facilities with limited access to emergency obstetric care (EmOC), and where the need for a C/S requires a time-consuming referral to a higher-level health facility, where the safety of a C/S cannot be guaranteed. In these settings, AVB can be a life-saving intervention for mothers and babies who are facing second stage complications.”2
“The WHO and other UN agencies have included AVB as one of the seven critical signal functions of basic EmOC, and one of the nine signal functions of comprehensive EmOC. However, reports indicate that, in most Low- and Middle-Income Countries, AVB is the least likely function to be performed in primary care facilities.”2
“The main barriers to the success of interventions to increase AVB use are related to healthcare professionals, environmental factors, and training. One of the main barriers reported…was the difficulty in ensuring that the staff acquired and maintained all necessary skills to conduct AVB over time, including obstetrics clinical skills (correct diagnosis for the need to conduct an AVB), technical skills to safely use the instrument and non-technical skills (communication with the woman and team).”2
“Additional barriers were the lack of continued hands-on supervision and practice, lack of institutional support for instrumental births, lack of skilled personnel (staff shortage, high turnover, need for retraining) and instruments, insufficient pain relief for women and fear of malpractice litigation in case of adverse outcomes. The main enablers to the success of the interventions included issues related to multidisciplinary training, clarity of the roles of healthcare providers, availability of trained and skilled healthcare professionals, and involving women in decision-making.”2
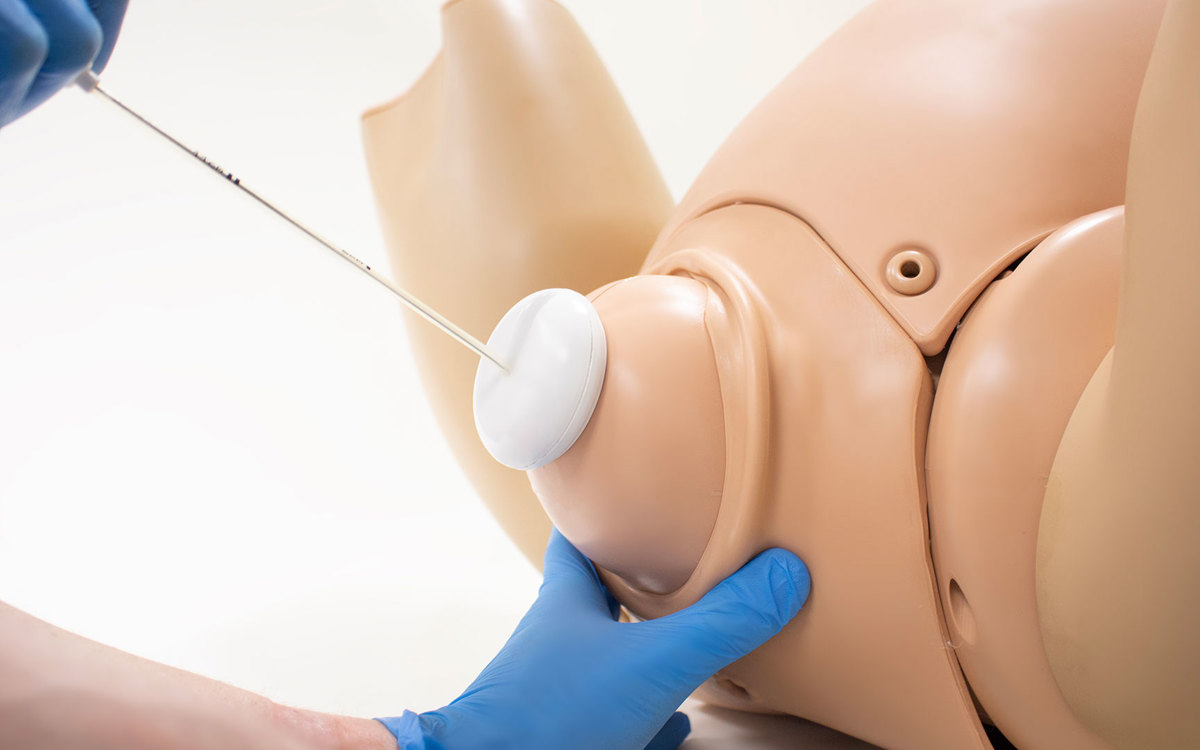
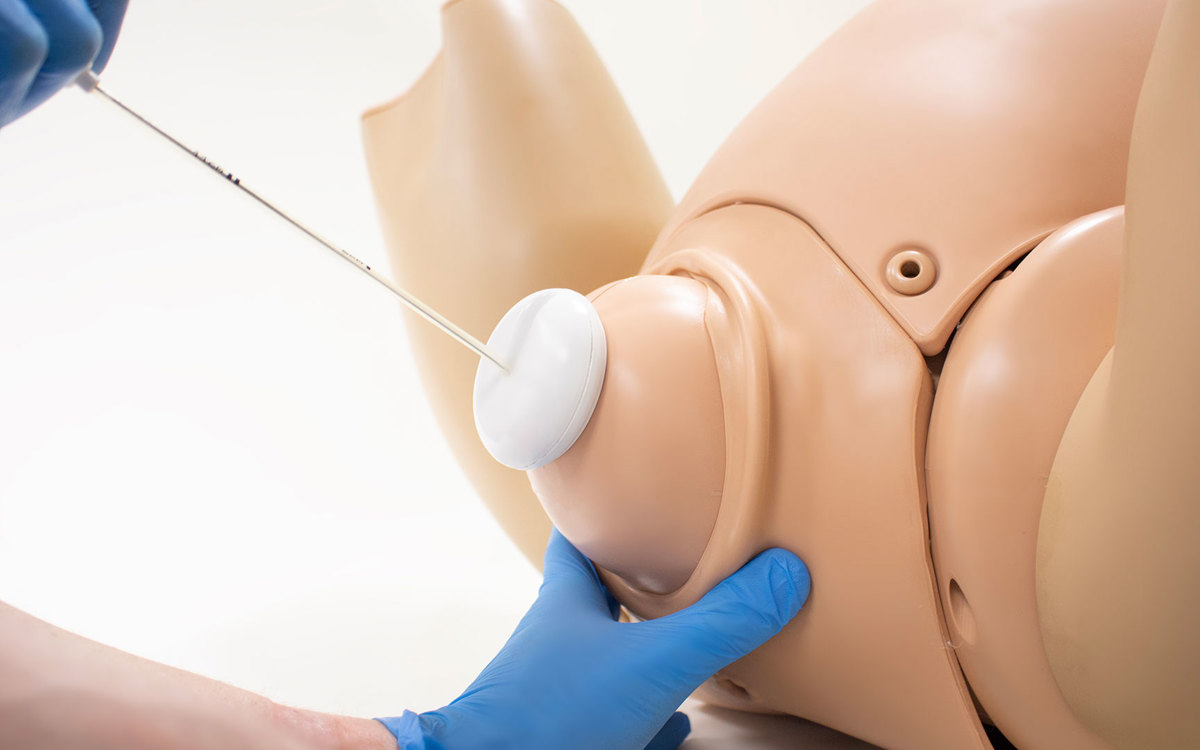
A new device for AVB currently under investigation is called the OdonAssist™ inflatable device. “The mechanism of the OdonAssist™ is based on inflating an air chamber around the fetal head to act as an anchor point, allowing the practitioner to apply traction.”3 A recent UK trial sponsored by the National Health System (NHS) “demonstrated that the OdonAssist™ could be successfully used with and without regional anaesthesia, in all occipito-anterior, occipito-transverse & occipito-posterior positions and that it is safe for mothers and infants. Because of its innovative mechanism of action, the OdonAssist™ does not cause typical bruising patterns on the fetal head, as is the case with forceps and ventouse. Additionally, satisfaction of both mothers and health professionals with the use of the device has been very high.”3
Limbs & Things is proud to offer a new Assisted Vaginal Birth module for the Birthing Simulator – PROMPT Flex range of products. This module includes realistic anatomy for placement and use of forceps, vacuum (or ventouse), and the OdonAssist™ device for safe vaginal deliveries that avoid unnecessary Cesarean Sections. We support the use of deliberate practice in a safe environment with our products to build both competence and confidence in providers globally. If you would like more information about the AVB module, don’t hesitate to reach out to us.
1 Assisted Vaginal Delivery, Indications, Management, Maternal-Fetal Complications
2 Interventions to Reintroduce or increase assisted vaginal births
3 Generating clinical evidence for an innovation in maternal and newborn health: The OdonAssist™
Did you like this article?
Share it on social media today, and remember to tag us!