













Clinical Male Pelvic Trainer (CMPT) Mk 2 - Advanced (Light Skin Tone)
Skin Tone
Model
Adding to cart...
Added to cart
Sorry, something went wrong adding the product to the cart.
The anatomically accurate Clinical Male Pelvic Trainer (CMPT) is the ideal platform to teach hands on male pelvic examinations. As well as the normal male anatomy, the Advanced model comes with 6 pathological penile modules for a varied learning experience.
What modules are included in the male examination range, and what do they represent?
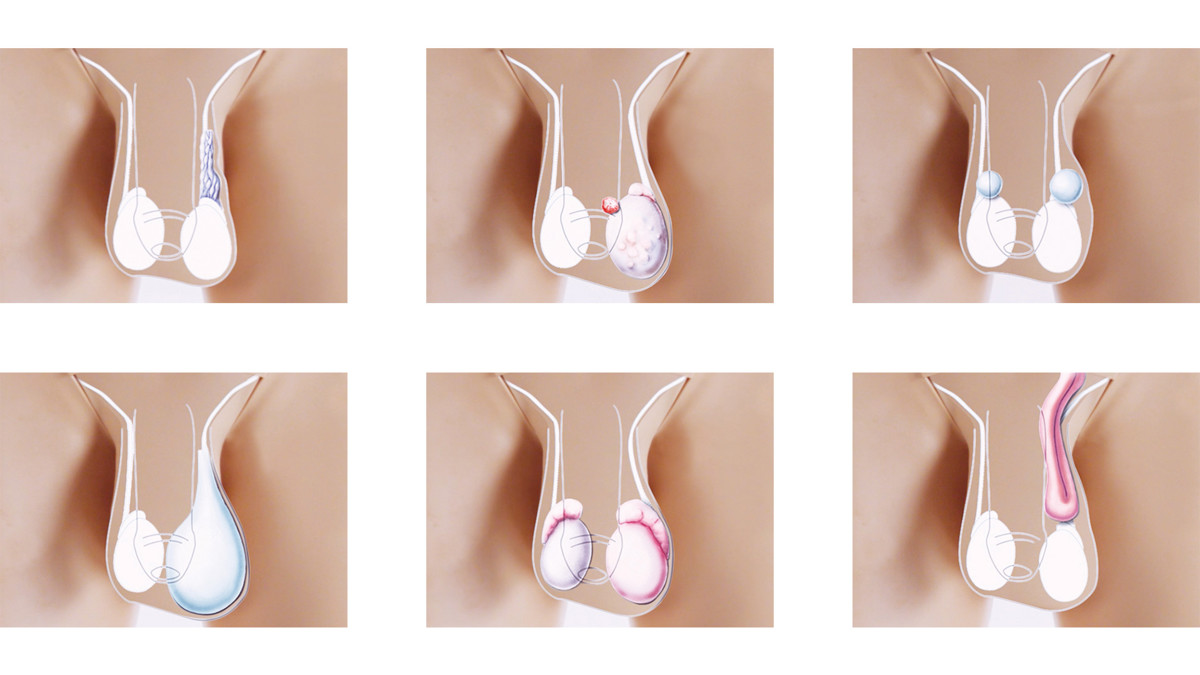
Module 1 – Normal anatomy: Representation of a healthy adult male
Module 2 – Varicocele: Visible or palpable enlarged veins ascending from the testicle
Module 3 – Testicular Tumour (Teratoma) and Penile Cancer: Solid mass within the left testicle and within the glans of the penis
Module 4 – Epididymal Cysts: Bilateral cysts at the head of the epididymis
The anatomically accurate Clinical Male Pelvic Trainer (CMPT) is the ideal platform to teach hands on male pelvic examinations. As well as the normal male anatomy, the Advanced model comes with 6 pathological penile modules for a varied learning experience.
What modules are included in the male examination range, and what do they represent?
Module 1 – Normal anatomy: Representation of a healthy adult male
Module 2 – Varicocele: Visible or palpable enlarged veins ascending from the testicle
Module 3 – Testicular Tumour (Teratoma) and Penile Cancer: Solid mass within the left testicle and within the glans of the penis
Module 4 – Epididymal Cysts: Bilateral cysts at the head of the epididymis
Module 5 – Hydrocele: Accumulation of fluid around the testis
Module 6 – Epididymitis/Epididymo-orchitis: Enlarged and nodular appearance of epididymis, and enlarged testis and epididymis
Module 7 – Indirect Inguinal Hernia: Enlarged scrotal sac because of the intruding small bowel
All aspects of male genital examination can be performed on this simulator:
- Inspection – Level, swelling, oedema and masses or the testes, pulling back of the foreskin to assess for penile cancer
- Palpation – feeling the inferior, middle and superior parts of testes, detecting the superior and inferior poles of the epididymis, and feeling the neck of the scrotum with thumb anteriorly and index finger posteriorly
This trainer was developed in collaboration with experts from:
- The Clinical Skills Resource Centre, University of Liverpool, UK
- Imperial College, London, UK
- Guy's Hospital, London, UK
- Southmead Hospital, Bristol, UK
- University of Southampton, UK
Reference: Journal of Surgical Education, Volume 74, Issue 3, May-June 2017
"Our study demonstrates that the CMPT MK 2—Advanced models have high “face validity” and may be a valuable tool for surgical education. The use of these models should be explored for use in the curriculum at medical school."
Overview
- Anatomically accurate male simulator that allows for realistic practice of the male pelvic exam
- 7 supplied modules give a wide variety of pathologies to identify
- A Foreskin Pack is included to practice procedures on both circumcised and uncircumcised anatomy
Realism
- Soft tissue genitals and abdominal wall
- Clear anatomical landmarks allow for a realistic palpation experience
- Penis, foreskin and scrotum respond in a life-like way under examination, adding realism
Versatility
- Allows training of male pelvic exam in both standing and supine positions
- CMPT modules are quick and easy to change
Cleaning
- Clean product surfaces with a soft damp cloth, warm water and mild detergent, after every training session
- Allow to dry thoroughly before storing
Safety
- External surfaces are latex free
- Interior anatomy of Module 5 (Hydrocele) and Module 7 (Indirect Inguinal Hernia), contain latex
- Only use water-based lubricant on the CMPT range
- Lubricate the foreskin before attaching it to the training module
- Do not leave foreskin on the model when not in use
- Wear gloves when handling the simulator, sharp surfaces such as jewellery and fingernails can damage silicone parts
Simulated Patient
- The Clinical Male Pelvic Trainers can be used with a simulated patient
Anatomy
Anatomy of the groin:
- Anterior Superior Iliac Spine (ASIS)
- Pubic symphysis and tubercles
Anatomy of male genitalia:
- Penis with attachable foreskins to simulate circumcised and uncircumcised anatomy
- Scrotum containing testicles with epididymis and vas deferens
Pathological representations of:
- Testicular tumour and penile cancer
- Epididymal cyst
- Varicocele Orchitis/Epididymo-orchitis
- Hydrocele
- Indirect Inguinal Hernia
Skills Gained
- Correct examination procedure of the male pelvis
- Dry catheterization
- Professional-to-patient communication
Examination and evaluation of:
- Normal anatomy
- Testicular abnormalities and penile cancer
- Abdominal and pelvic pain
Product Contains

ART Mat for CMPT
-
Light
-
Dark

CMPT Mk 2 Module 1: Normal (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 2: Varicocele (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 3: Tumors (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 5: Hydrocele (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 6: Epididymitis/Epididymo-orchitis (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 7: Indirect Inguinal Hernia (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Abdominal Insert (Light Skin Tone)

CMPT Mk 2 Pubic Bone
-
Light
-
Dark

CMPT Mk 2 Foreskins (Pack of 2, Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 4: Epididymal Cysts (Light Skin Tone)
Comparison |
Model |
|
|---|---|---|
| What's included | Std | Adv |
| ART Mat for CMPT | No | Yes |
| CMPT Module 1: Normal | Yes | Yes |
| CMPT Module 2: Varicocele | No | Yes |
| CMPT Module 3: Tumors | No | Yes |
| CMPT Module 4: Epididymal Cysts | No | Yes |
| CMPT Module 5: Hydrocele | No | Yes |
| CMPT Module 6: Orchitis/Epididymo-orchitis | No | Yes |
| CMPT Module 7: Indirect Inguinal Hernia | No | Yes |
| CMPT Abdominal Insert | Yes | Yes |
| CMPT Pubic Bone | Yes | Yes |
| CMPT Foreskins Pack (contains 2 foreskins & 3 lubricant sachets) | Yes | Yes |
| Lower torso | Yes | Yes |
| Support Base | Yes | Yes |
| Carry case (trainer) | Yes | Yes |
| Carry case (modules) | No | Yes |
Works with the following products:
-
Light
-
Dark

CMPT Mk 2 Module 1: Normal (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 2: Varicocele (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 3: Tumors (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 4: Epididymal Cysts (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 5: Hydrocele (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 6: Epididymitis/Epididymo-orchitis (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Module 7: Indirect Inguinal Hernia (Light Skin Tone)
-
Light
-
Dark

CMPT Mk 2 Abdominal Insert (Light Skin Tone)

CMPT Mk 2 Pubic Bone
-
Light
-
Dark

CMPT Mk 2 Foreskins (Pack of 2, Light Skin Tone)
References
National Organisation of Nurse Practitioner Faculties, Nurse Practitioner Core Competencies Content, 2017 Independent Practice Competencies p.14 3.b Uses advanced health assessment skills to differentiate between normal, variations of normal and abnormal findings. 3.c Employs screening and diagnostic strategies in the development of diagnoses.
AAFP Recommended Curriculum Guidelines for Family Medicine Residents, Men’s Health Reprint No. 257, 2016 p.3 Perform a comprehensive male physical examination, including urogenital... p.5 the resident should demonstrate the ability to independently perform or appropriately refer the following: 1. Male-specific examination a. Penile/testicular/scrotal exam c. Hernia/inguinal exam
AAMC (2008) - Recommendations for Pre-clerkship Clinical Skills Education for Undergraduate Medical Education p.26Appendix 5: Patient Examination. Perform testicular exam and describe examination process and findings
CPMEC Australian Curriculm Framework for Junior Doctors v 3.1, 2012, p.7: History and Examination: Performs a comprehensive examination of all systems; Elicits symptoms & signs relevant to the presenting problem or condition. Discriminates between the possible differential diagnoses relevant to a patient's presenting problems or conditions
RACGP Curriculum for Australian General Practice 2016, SH16 Sexual and Reproductive Health Essential skills for general practitioners to develop and maintain include: ...undertaking a sensitive genital examination, if appropriate, to assess risk, determine appropriate assessment, investigation and management
Medical Deans' Clinical Assessment Blueprints for the medical graduate 4. Conducts ... organ(s)/system specific physical examination as appropriate. 5. Integrates the information obtained to arrive at an appropriate diagnosis and differential diagnosis.
Competence and Curriculum Framework for the Physician Assistant 2012, p 12 2.3.5 ...Perform a physical examination tailored to the needs of the patient and the demands of the clinical situation, including ...male uro-genital examination
Specialty Training Curriculum for Core Medical Training, 2013 p.86: Perform full examination including...scrotum, male urethra
The UK Foundation Programme Curriculum 2016. p.9: obtains history, performs clinical examination, formulates differential diagnosis and management plan (FPC 11)
The Intercollegiate Surgical Curriculum, Urology Surgery, Aug 2015 p.20 Recognise the common malignant and potentially malignant conditions of the penis...Diagnose and manage patients presenting with scrotal symptoms such as hydrocele, epididymal cyst, varicocele
Outcomes for Graduates 2018, General Medical Council, p.16 Diagnosis and medical management: 14b. safely and sensitively undertake an appropriate physical examination ...interpret findings from physical examinations...synthesise findings from the history, physical and mental state examinations and investigations ... and make proposals about underlying causes or pathology
RCN Competencies - Advanced Nurse Practitioners, 2012, p.4 ...receiving patients with undifferentiated and undiagnosed problems and making an assessment of their health care needs, based on highly-developed nursing knowledge and skills ... such as physical examination
Guidance for Satisfactory Progression at ARCP panels for GP Specialty Trainees, 2016 p.6 ... evidence of competence of intimate examinations which includes ...the full range of ... male genital examinations.
Can trainees practice catheterization on the Clinical Male Pelvic Trainer?
Yes, the CMPT can be used to practice dry catheterization techniques. However, if you’re looking to do more extensive training in this procedure, the Male Catheterization Trainer range may be more suited to your training needs.
Is it possible to use transillumination on the male pelvic simulator to identify pathologies?
Using the supplied LED Pen Torch, transillumination can be performed on the scrotum. For example, on Module 4, illuminating the scrotum will allow trainees to visually identify the two Epididymal Cysts.
Can the CMPT be used to simulate cancer in male genitalia?
Yes, Module 3 can be used in the identification of two presentations of cancer. The left testicle has a solid mass with an irregular surface, representing a Testicular Tumour or Teratoma. The penis has visual lesion, the lump is solid and has an irregular surface, representing Penile Cancer.












