The Impact of Midwifery on Maternal Mortality
Over the past few years, there has been a global focus on decreasing maternal mortality rates (MMR). So much emphasis has been placed on these often-preventable deaths that the World Health Organization (WHO) has called for a global target to increase equity in global MMR reduction.

The following goals, as outlined by the WHO are: “By 2030, all countries should reduce MMR by at least two thirds of their 2010 baseline level. The average global target is an MMR of less than 70/100,000 live births by 2030. The supplementary national target is that no country should have an MMR greater than 140/100,000 live births (a number twice the global target) by 2030.”1
So, can midwives help to achieve this target? “The Lancet Series on Midwifery (2014) sets out the evidence on the needs of women and their newborns. This evidence estimates that safe and effective midwifery care (which includes family planning) can avert 83% of all maternal deaths, stillbirths, and newborn deaths.”2
In 2013, the International Confederation of Midwifery Education (ICM) updated their global standards to “strengthen midwifery worldwide by preparing fully qualified midwives to provide high quality, evidence-based health services for women, newborns, and childbearing families.”3
“The potential impact of midwives who have been educated and trained and are regulated to provide the full scope of ICM competencies would be a rapid and sustained reduction in maternal and newborn mortality and morbidity. A recent Cochrane review, where a model of midwife-led continuity of care is in place in well-functioning midwifery systems, shows that 24% of preterm births can be prevented.”2
When comparing maternity care provided globally, it is easy to wonder if the MMR rate is lower in the countries that provide more comprehensive midwifery services. And, while the following graph is combined from different sources, even the least experienced researcher can see that where there is more nursing and midwifery care, the MMR is lower.
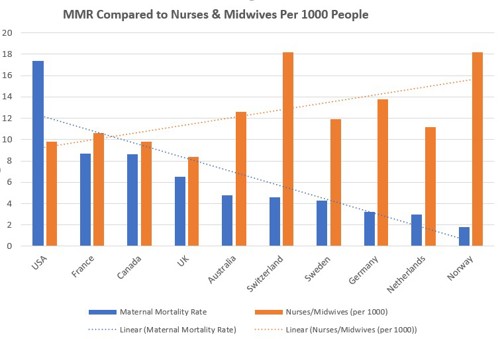
Other sources reference this same notion. In an article published in AJMC (2020), Melillo found that “When it comes to care providers, the United States and Canada ‘have the lowest overall supply of midwives and obstetrician-gynecologists (OB-GYNs) — 12 and 15 providers per 1000 live births, respectively,’ whereas all other countries have a supply that is between 2 and 6 times greater.
Midwives differ from OB-GYNs in that they help manage a normal pregnancy, assist with childbirth, and provide care during the postpartum period. In contrast, OB-GYNs are physicians trained to identify issues and intervene should abnormal conditions arise. OB-GYNs typically only provide care in hospital-based settings.
The role of midwives has been found to be comparable or preferable to physician-led care in terms of mother and baby outcomes and more efficient use of health care resources. WHO recommends midwives as an evidence-based approach to reducing maternal mortality.”5
One way to ensure midwives are trained an prepared for birthing scenarios is to utilize simulation. Visit our Birthing Simulator - PROMPT Flex to find out more.
References:
1. WHO: strategies toward
2. WHO: Strengthening Midwifery
3. ICM Global Standards
4. PEW Trusts: Rural America Has a Maternal Mortality Problem. Midwives Might Help Solve It
5. US Ranks Worst in Maternal Care, Mortality Compared with 10 other Developed Nations
6. NACPM Legal Recognition of CPM
7. WHO: Simulation in Nursing and Midwifery Education
8. Graph sources: Sources: EOCD, Commonwealth Fund, Statista, WHO Data/GHO/Indicators
Did you like this article?
Remember to share on social media and tag us!

